For people with chronic obstructive pulmonary disease (COPD), emphysema, pulmonary fibrosis and other chronic lung diseases, keeping a close eye on their blood oxygen level is typically part of the daily routine.
However, for people living with COPD and other chronic lung conditions, receiving enough oxygen can be challenging. Every cell, organ and tissue in your body needs adequate oxygen, so oxygen is essential to a properly functioning body.
When your body doesn’t receive enough oxygen, it’s unable to function properly.
We’re here to help you better understand your blood oxygen level, how your body gets oxygen and what it could mean for you.
Oxygen and the Body
Your body uses oxygen in various ways to keep you at your best. Your blood transports oxygen throughout your body. Your body contains many different types of blood vessels, which act as the road system for your blood to travel throughout your body.
Oxygen-rich blood travels through arteries and arterial branches to deliver oxygen and essential nutrients to your body. Capillaries are small, thin blood vessels that connect arteries and veins.
Capillaries are important because they allow oxygen, nutrients, carbon dioxide and waste to pass to and from the tissue’s cells. Oxygen-poor blood travels through veins back to the heart and lungs where it will be re-oxygenated.
Your heart and lungs work together to deliver oxygen to your body, and your lungs inhale oxygen-rich air and exhale carbon dioxide.
The heart pumps your blood to your lungs, so your blood can become oxygenated. Then, your heart pumps the oxygenated blood through your arteries and sends your blood to deliver oxygen to other cells, organs and tissues in your body.
How Your Heart and Lungs Deliver Oxygen Step-by-Step
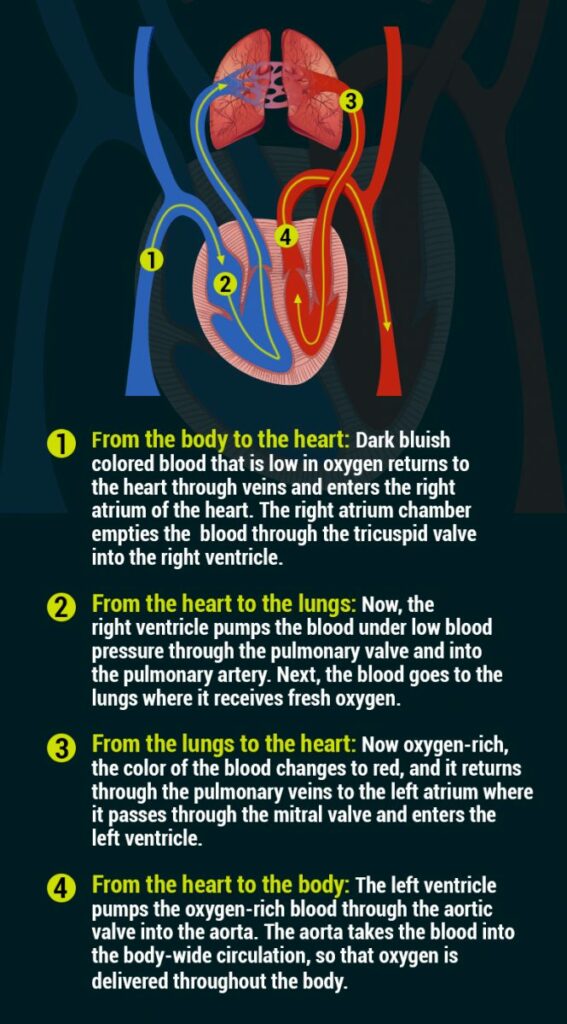
Your heart has four chambers and four valves, which work to pump blood throughout your body. Your lungs and linked blood vessels deliver oxygen and remove carbon dioxide.
The bronchi inside the lungs branch into smaller, thinner tubes called bronchioles. These tubes end in bunches of tiny, round air sacs called alveoli. Alveoli are covered in capillaries, and these capillaries connect to a network of veins and arteries.
The pulmonary artery and its branches deliver oxygen-poor blood to the capillaries that surround the air sacs. Once inside the air sacs, carbon dioxide moves from the blood and into the air to be exhaled while oxygen moves from inhaled air into the capillaries.
Oxygen-rich blood then travels to the heart through the pulmonary vein and its branches, and on to the rest of the body.
Here’s How Oxygen Is Moved Through the Heart and Lungs to the Body:
Your Blood Oxygen Level and What It Means
A healthy, normal blood oxygen level remains around 95 percent to 100 percent. You can monitor your blood oxygen level at home with a pulse oximeter. Values below 90 percent are considered low.
When your body doesn’t receive enough oxygen and you have a low blood oxygen level, hypoxemia or hypoxia, cyanosis and other conditions may occur.
Because COPD and other chronic lung diseases restrict or obstruct normal breathing, low blood oxygen levels can be a serious issue. Hypoxemia or hypoxia occurs when your body has insufficient oxygen and can range from mild to severe.
Symptoms of hypoxia can include severe shortness of breath, wheezing, constant coughing, a choking feeling and a bluish discoloration of the skin (cyanosis).
Chronic hypoxia can lead to cerebral hypoxia or brain hypoxia, which means that your brain cells could become seriously damaged within minutes.
If you suspect hypoxia call your doctor immediately. For cerebral hypoxia, call 911.
Improve Your Blood Oxygen Level
Many doctors will prescribe oxygen therapy to help you receive enough oxygen and to improve your blood oxygen levels. Your doctor may also prescribe breathing exercises, diet and exercise changes, pulmonary rehabilitation and medications to help you breathe.
Keeping a close eye on your blood oxygen level is important as well. Remember to see your doctor regularly even if you’re feeling well, so you and your doctor can work together.

Christine Kingsley, APRN is the Health and Wellness Director at the Lung Institute where she focuses on providing helpful online resources for people looking for information on various lung diseases, breathing exercises, and healthy lifestyle choices. She advocates for holistic care that involves working with your doctor to explore all options including traditional and alternative care while focusing on diet and exercise as proactive measures.









