Pneumonitis is a term to describe the inflammation of lung tissue. Inflammation can play a major in almost any lung disease.
When patients with COPD experience a flare-up in symptoms, the culprit can usually be found in the trigger of inflammation to the lungs or airways. Sufferers of pulmonary fibrosis know this all too well with lung scarring.
What you may not have known is that different toxins can cause inflammation within the body.
Where Do The Toxins Come From?
There are two different types of inflammation, acute and chronic. Acute inflammation is the body’s natural response to tissue damage and usually lasts for a short period of time. Chronic inflammation is the tricky one.
With this form of inflammation, your body isn’t exactly sure what to do. Your immune system will respond to various factors and, most of the time, cannot figure out the difference between healthy cells or foreign invaders.
With the case of lung disease, inflammation can occur from several factors, including toxins that we take in. Fear not! Most of these toxins are within our control and can be avoided! Here is a list of some of the harmful toxins that impact us:
- Poor Diet – Eating processed foods, too many animal products, sugary drinks, excess alcohol and more can all cause unwanted toxins to enter the body. Knowing which ones cause your inflammation will help to avoid additional flare-ups.
- Food Allergies – Knowing which foods you are allergic to will reduce the chance of increased inflammation.
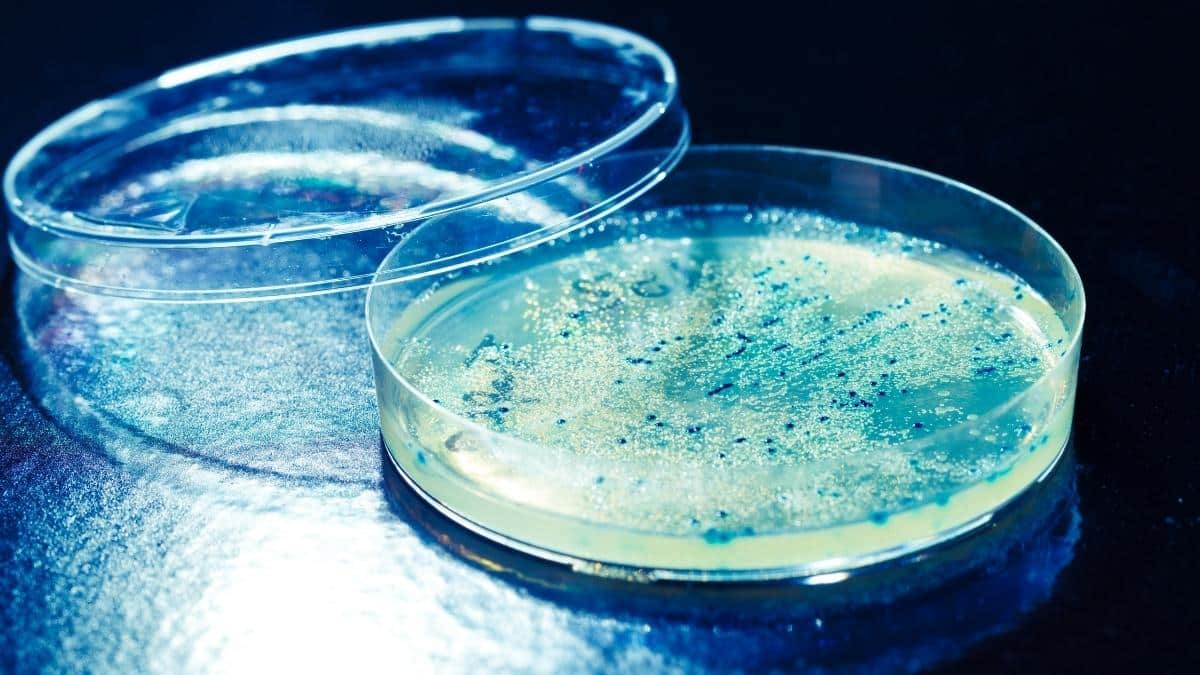
- Chronic Infections – Bacteria, viruses, yeast and parasites can each cause inflammation. Having a simple cold or stomach cramp can contribute to inflammation. Be sure to stay healthy and talk to your doctor if you are experiencing an infection.
- Smoking – Smoking or breathing in cigarette smoke can lead to inflammation of the lung tissue and damage the airways.
- Stress and exhaustion – Being stressed out is its own form of toxin. The body produces a chemical which is meant to make us relax and calm down from stress, but too much of it can actually be damaging.
Recent Updates
Scientists at the University of Texas Health Science Center in San Antonio released a new study describing a bacterial toxin that might contribute to the inflammation of several pulmonary conditions.
Researchers listed that this new toxin could lead to asthma development and potentially impact the flare-up symptoms of lung diseases such as COPD and Sarcoidosis.
The bacteria toxin, called M pneumoniae, is a common and persistent infection in the lungs and airway. Once the infection is present, it creates a toxin (CARDS) that reacts with a key molecule within the inflammatory pathways known as NALP3.
When these two conditions combine, it causes inflammation to occur throughout the lungs. The CARDS toxin is considered to be the first major bacterial respiratory toxin discovered since the days of diphtheria and pertussis.

Christine Kingsley, APRN is the Health and Wellness Director at the Lung Institute where she focuses on providing helpful online resources for people looking for information on various lung diseases, breathing exercises, and healthy lifestyle choices. She advocates for holistic care that involves working with your doctor to explore all options including traditional and alternative care while focusing on diet and exercise as proactive measures.