If you live with pulmonary fibrosis, you’ve likely heard a lot about the scarring of the lungs.
People with pulmonary fibrosis develop scar tissue in their lungs, which makes it difficult to breathe normally and fully.
Let us explain what it means to have scarring of the lungs and pulmonary fibrosis.
What Is Pulmonary Fibrosis?
Pulmonary fibrosis is a condition that causes your lung tissue to become thickened and scarred. This makes it more difficult for air to pass between the walls of the lungs and into the body. The name itself is quite accurate, as pulmonary refers to your lungs and fibrosis means “scarring.”
Once the scarring of the lungs occurs, unfortunately there is no way to reverse the process. Pulmonary fibrosis can lead to other medical problems, such as a collapsed lung, lung infections, blood clots in the lungs and lung cancer.
In time, pulmonary fibrosis can lead to respiratory failure, pulmonary hypertension and heart failure. Because of this, managing the disease is imperative.
Disease management is not only preventative, but also helps the person with pulmonary fibrosis enjoy a higher quality of life.
You might also hear the term idiopathic pulmonary fibrosis, which refers to pulmonary fibrosis with no known cause. In fact, in most pulmonary fibrosis cases, the exact cause is unknown, although we can speculate different reasons as to why a person might develop the disease.
What Are Symptoms Of Pulmonary Fibrosis?
Pulmonary fibrosis can develop either very quickly or very slowly – it various from person to person. In most cases, a person’s breathing will become increasingly difficult over time.
Below are the primary symptoms of pulmonary fibrosis:
- Shortness of breath, especially after exertion
- Dry, hacking cough
- Fast, shallow breathing
- Gradual, unintended weight loss
- Fatigue
- Aching joints and muscles
- Widening and rounding of the fingers and toes, also referred to as “clubbing”
What Causes Pulmonary Fibrosis?
Most cases of pulmonary fibrosis unknown, meaning there is no known cause for the disease. However, there are factors that may increase the risk of pulmonary fibrosis, which include the following:
- Smoking cigarettes
- Viral infections
- Exposure to environmental irritants, such as gases, fumes, pollutants and workplace hazards
- Certain medications
- Genetics
- Gastroesophageal reflux disease (GERD), a condition in which acid from your stomach backs up into your throat
How is Pulmonary Fibrosis Diagnosed?
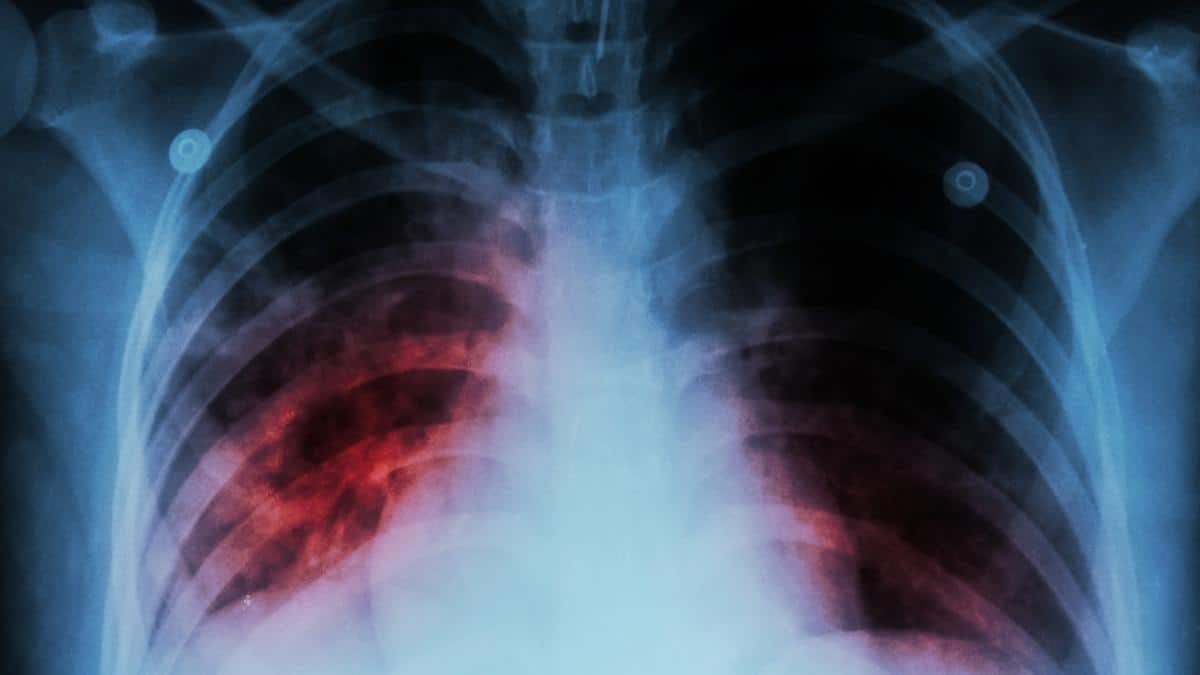
Pulmonary fibrosis is an interstitial lung disease, which refers to any condition that causes progressive scarring of the lungs and its tissues. If your doctor suspects that you may have pulmonary fibrosis, he or she will likely refer you to a lung specialist.
Here are some tests that are used to detect pulmonary fibrosis:
- Chest X-ray
- Breathing tests to understand the extent of the damage
- Blood tests to check for oxygen levels in the bloodstream, autoimmune disease and possible infections
- High resolution CT scan of chest, referred to as HRCT
- Lung biopsy
- Exercise test
What are my Treatment Options for Pulmonary Fibrosis?
There is currently no known cure for pulmonary fibrosis. However, there are steps that can be taken to manage the symptoms and improve a patient’s quality of life.
The goals of treatment are to hopefully slow the progression of the disease, reduce symptom flare-ups and help the person with pulmonary fibrosis to live an active and healthy life.
Below are the main treatment options for pulmonary fibrosis:
Medications
Many people with pulmonary fibrosis are prescribed a corticosteroid, such as prednisone, to reduce inflammation in the lungs. However, corticosteroids can have some negative side effects, particularly when taken over a long period of time.
Because of this, the use of corticosteroids needs to be monitored very closely. Other potential medications that reduce inflammation include azathioprine and cyclophosphamide, both of which suppress the immune system.
FDA-approved drugs for pulmonary fibrosis are nintedanib (Ofev®) and pirfenidone (Esbriet®, Pirfenex®, Pirespa®).
Supplemental Oxygen
Supplemental oxygen helps ensure that your body is receiving enough oxygen. Some people use supplemental oxygen 24 hours a day, while others use it only as needed.
Pulmonary Rehabilitation
Pulmonary rehabilitation is a program that teaches you about your disease, how to exercise and manage symptoms and often includes support and counseling.
Pulmonary rehabilitation can be a great way to deal with the mental impact that the disease has on a person as well.
Lung Reduction or Transplant
In more severe cases, a lung reduction or transplant might be an option. However, not everyone is eligible because the surgery is hard on the body.
A person needs to be in good physical condition, have no other life-threatening illnesses and be willing to undergo subsequent medical treatment to be considered for a lung transplant.
Another thing to keep in mind is the prognosis for a lung transplant. The five-year survival rate is roughly 50 percent.

Christine Kingsley, APRN is the Health and Wellness Director at the Lung Institute where she focuses on providing helpful online resources for people looking for information on various lung diseases, breathing exercises, and healthy lifestyle choices. She advocates for holistic care that involves working with your doctor to explore all options including traditional and alternative care while focusing on diet and exercise as proactive measures.