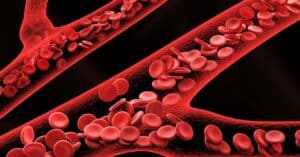
Your oxygen level refers to the amount of oxygen in your blood. When that number drops below normal levels, it’s referred to as hypoxemia.
People with lung conditions such as chronic obstructive pulmonary disease, or COPD, need to be particularly aware of their blood oxygen levels, as they are at a higher risk of hypoxemia.
Tools like pulse oximeters, a small device that attaches to your finger, help you to better understand blood oxygen levels in your body.
For those who use supplemental oxygen, a pulse oximeter is a valuable tool in measuring your oxygen saturation level, helping you to understand when to use supplemental oxygen.
So, at what point do oxygen levels go from being normal to unsafe? Before we dive into that more, let’s first explore what it means to have a normal oxygen level and a low oxygen level.
What is a Normal Oxygen Level?
Most people with COPD have oxygen levels that are below normal, even when using supplemental oxygen. The best way to measure oxygen level is through arterial blood gases (ABGs), measured in millimeters of mercury, or mm Hg.
In the blood, a normal oxygen level typically range from 75 to 100 mm Hg. When blood oxygen levels drop under 60 mm Hg, it is usually an indication that the person needs supplemental oxygen.
If you have COPD, your doctor might give you a prescription for supplemental oxygen to help you to maintain normal oxygen levels.
Your doctor should give you a safe range that he or she wants you to stay within to help you better understand when to use the supplemental oxygen.
If you find that you’re consistently falling below the range that your doctor suggested, notify your doctor immediately, as your doctor may need to adjust the oxygen flow rate on your supplemental oxygen.
Maintaining a normal oxygen level is imperative for effectively managing COPD.
Your doctor might also give you specific directions to adjust your own oxygen flow rate based on your oxygen saturation levels. Consult with your primary care doctor or pulmonologist for the best plan of action for your specific situation.
What is a Low Oxygen Level, or Hypoxemia?
When you don’t get enough oxygen in your blood, the body has trouble effectively nourishing your cells, tissues and organs. A low blood oxygen level, or hypoxemia, can occur suddenly, or can also take place over time.
Frequently, for people with COPD, low oxygen levels occur over time. Doctors often prescribe supplemental oxygen to COPD patients with hypoxemia.
Many people with COPD, however, are not aware that they are hypoxemic. Hypoxemia with COPD can result in a reduction in quality of life, impaired skeletal muscle function, decreased exercise tolerance and increased risk of death.
Because of this, it’s important to be able to recognize the signs and symptoms of hypoxemia with COPD:
- Confusion
- A sense of euphoria
- Restlessness
- Headache
- Shortness of breath
- Rapid breathing
- Dizziness, lightheartedness and/or fainting spells
- Lack of coordination
- Rapid heart rate
- Elevated blood pressure
- Visual disturbances
- Bluish tint to lips, earlobes and/or nail beds
- Elevated red blood cell count or polycythemia
Monitoring your Oxygen Levels
While the best way to monitor blood oxygen levels is through your ABGs, they are difficult to measure from home. The best way to measure oxygen levels at home is to use a pulse oximeter, which measures oxygen saturation.
Normal oxygen saturation levels range from 95 to 100 percent. Anything under 90 percent is considered low. In general, anyone having levels below 90 percent at rest should explore their options for supplemental oxygen therapy with their primary care doctor.
If you or a loved one is experiencing low oxygen levels, contact your primary care physician immediately to discuss your treatment options.

Christine Kingsley, APRN is the Health and Wellness Director at the Lung Institute where she focuses on providing helpful online resources for people looking for information on various lung diseases, breathing exercises, and healthy lifestyle choices. She advocates for holistic care that involves working with your doctor to explore all options including traditional and alternative care while focusing on diet and exercise as proactive measures.