What Is Bronchiectasis?
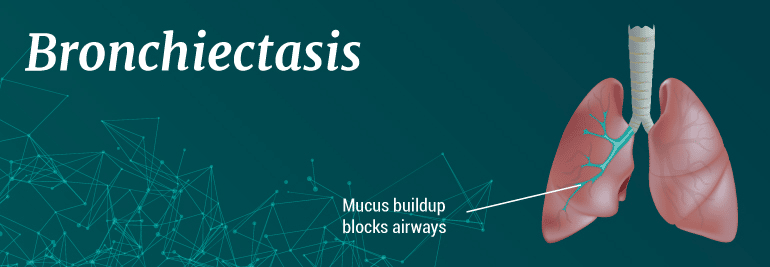
Bronchiectasis is a pulmonary condition in which damage to the airways causes them to widen and become scarred. The lung disease causes your airways to slowly lose their ability to clear out mucus.
As a result, the mucus continues to build up creating a mucus blockage, which allows bacteria to continually grow. This often results in repeated lung infections. The blockage and accompanying infections cause inflammation, which lead to weakened air passages and difficulty breathing.
Over time, the airways will lose their ability to move air in and out. This can prevent a sufficient amount of oxygen from reaching vital life-sustaining organs.
Bronchiectasis is a progressive inflammatory lung disease, which means that it typically worsens with time. That also means that there is currently no cure for bronchiectasis, though there are many treatments that can help make the symptoms of this condition more manageable. Because this is a progressive condition, the key to treating bronchiectasis effectively is early diagnosis.
If you suspect that you or a loved one may have bronchiectasis, read through the symptoms and information listed in this article.
Symptoms of bronchiectasis
The symptoms associated with bronchiectasis can vary from person to person, but they most often include the following:
- Daily coughing up yellow or green mucus
- Shortness of breath
- Chronic fatigue
- Fevers and/or chills
- Wheezing
- Coughing up blood or mucus mixed with blood
These symptoms act as early indicators that you may have bronchiectasis. If you are experiencing these symptoms, even if it is just one symptom regularly, you should schedule an appointment with your doctor immediately to diagnose your condition. If it turns out that your symptoms are a result of bronchiectasis, your doctor can help you choose the right treatment options for your condition.
Causes of bronchiectasis
There are many factors that can contribute to the development of bronchiectasis. Unlike other forms of chronic lung disease, the causes of bronchiectasis are not often linked to lifestyle habits such as smoking. In fact, they are more often linked to the genetics and immune system.
Some of the most common causes of bronchiectasis include:
- Humoral immunodeficiency
- Inflammatory bowel disease
- Rheumatologic diseases
- Alpha1-antitrypsin deficiency
- Chronic obstructive pulmonary disease (COPD)
- HIV infection
- Allergic bronchopulmonary aspergillosis
Bronchiectasis is a disease that doesn’t discriminate. Both women and men can develop bronchiectasis, but women have a higher risk of development. Overall, two-thirds of individuals with bronchiectasis are women.
Non-congenital bronchiectasis typically affects adults and older children. It is significantly more common than the congenital type, which only affects children.
If you have been diagnosed with one of these bronchiectasis causes, and you are experiencing any of the symptoms listed above, you should contact your doctor immediately to schedule an appointment to diagnose the cause of your symptoms.
Diagnosing bronchiectasis
When you go in for your doctor’s appointment to confirm whether or not you have bronchiectasis, you can expect the following diagnostic tests. First, the doctor will likely ask you about your medical history, as well as your family’s medical history. Since bronchiectasis is closely linked to other medical conditions, it’s important for your doctor to be aware of your medical history in order to make an accurate diagnosis.
Once you have this conversation, your doctor may perform a physical examination, as well as a pulmonary test. A pulmonary test is a simple test that requires you to blow into a special mouthpiece. This mouthpiece is designed to gauge your lung strength and capacity, which is used to score your overall pulmonary function.
In some cases, your doctor may recommend X-rays and lab work before he/she confirms a bronchiectasis diagnosis. Once your diagnosis is confirmed, you can begin a treatment plan.
Treatment options for bronchiectasis
There is no cure for bronchiectasis. It is a progressive condition that may continue to worsen over time. However, there are many treatment options available to help you manage your symptoms, and some treatment options that may help slow the progression of your condition.
While traditional treatments for bronchiectasis include an inhaler, medication and oxygen therapy, regenerative treatments use the cells in a patient’s own body to help target and reduce the inflammation in the lungs. Traditional treatments play a very reactive role in treating bronchiectasis; they are only useful when symptoms are occurring. However, regenerative treatment aims to reduce the occurrence of symptoms altogether.
