With all of the numbers, facts, and information you have to remember about chronic obstructive pulmonary disease (COPD), you may have many questions.
One common question is, “how long can I expect to live with COPD?”
The life expectancy of people diagnosed with COPD (chronic obstructive pulmonary disease) reduces significantly over time. The period varies by gender, disease stage, and whether they’ve ever smoked, are still smoking, or stopped smoking.
Studies show males aged 65 with Stage 3 or 4 COPD reduce their life expectancy by nearly six years. Conversely, males of the same age group with Stage 1 COPD who are still smoking reduce their life expectancy by 0.3 years, and those with Stage 2 COPD reduce it by two years.
Here’s what you need to understand about COPD life expectancy and how doctors can predict what your prognosis could be and even options to extend your life.
Understanding COPD and Your Life Expectancy
COPD is an abbreviation for chronic obstructive pulmonary disease, a group of diseases that affects the lungs. The condition results from prolonged exposure to irritating gases like smoke which block the airways, causing breathing problems.
People with COPD often wheeze, cough, produce excessive mucus, and experience difficulty breathing. They’re also more likely to develop lung cancer, and heart disease, among other diseases. Two conditions are believed to contribute to COPD:
Chronic Bronchitis:
The condition causes inflammation in the lining of bronchial tubes, which are responsible for carrying air to and from the alveoli. Chronic bronchitis damages the cilia (the hair-like fibers lining the bronchial tubes), which help eliminate mucus.
As a result, it becomes more challenging to remove mucus, making you cough more. That’s why people with chronic bronchitis develop mucus that lingers for an extended period, sometimes up to two years. Other symptoms of chronic bronchitis are shortness of breath and coughing.
Emphysema:
The condition develops when the alveoli are destroyed, causing them to merge into one large air sac. Since it doesn’t absorb oxygen as well as healthy alveoli, the blood gets less oxygen.
Emphysema also causes the lungs to stretch out, losing their elasticity. As a result, air remains trapped in the lungs, making breathing difficult.
Is COPD Considered a Terminal Illness?
COPD is a terminal illness that progresses over time. Since there’s no cure for the disease, treatment can only manage its symptoms.
Also, diagnosing the condition in its early stages and administering medical treatment immediately slows down the speed at which the symptoms progress.
With the proper treatment, one’s life expectancy may increase by 10-20 years after diagnosis.
What Is the Most Common Cause of Death in COPD?
Death in COPD often results from respiratory complications, which is common in patients in Stage 4 of the illness. However, mortality in patients with mild to moderate COPD is due to lung cancer and cardiovascular disease.
Treatment may relieve pain and discomfort at this stage, but it won’t be as helpful as in the earlier COPD stages. Patients can only rely on palliative care options to manage the condition.
This means:
- Performing mind-body therapies like yoga
- Getting help with daily chores
- Taking medication for depression, anxiety, and other such conditions
- Performing complementary therapy like massage therapy
How Fast Does COPD Progress?
COPD progresses slowly, sometimes causing a delay in accurate diagnosis until late in its stages. Its progression varies by person, stage, and group of the illness.
A diagnosis helps determine COPD by group and stage and enables the doctor to prescribe the best treatment.
When the doctor classifies COPD by stage, it’s diagnosed as a Stage 1, 2, 3, or 4 – the higher the stage, the more advanced the condition.
The doctor may also classify COPD by group, i.e., Group A, B, C, or D. This classification is based on the severity of the symptoms, the number of flare-ups experienced in the last 12 months, and hospitalizations required.
Based on this criterion, COPD patients will be in groups A, B, C, or D.
This means:
- Groups A and B: COPD patients in this group have few symptoms and have experienced 0-1 exacerbations in the last year without getting hospitalized.
- Groups C and D: These patients have experienced two or more COPD flare-ups and have been hospitalized one or more times.
Patients who fall into GOLD Stage 1 and Group A don’t progress to clinically severe COPD rapidly, even when they continue smoking. In fact, they exhibit similar respiratory symptoms as smokers with normal spirometry results.
However, COPD in advanced stages like GOLD Stage 3 and Group C and D progresses quickly if the patient continues smoking and doesn’t seek urgent medical attention.
What Makes COPD Progress Faster?
Smoking will make COPD progress faster even when the patient is taking medication. That’s because continued smoking renders the drugs ineffective, causing the condition to progress to more severe stages.
Also, not taking medication as prescribed may cause COPD to progress faster.
Does COPD Progress After Quitting Smoking?
Smoking cessation may alter the progression of COPD. Studies show that COPD patients who stop smoking experience improved respiratory symptoms, reduced lung inflammation, and loss of pulmonary function.
Quitting smoking also helps manage other illnesses like heart disease and heart disease resulting from COPD.
Lung Cancer and COPD
Lung cancer and COPD are closely related. A 2012 review article discussing the relationship between the two conditions found that 1% of people with COPD developed lung cancer yearly.
Both conditions also share several factors:
Inflammation:
Lung cancer and COPD cause long-term inflammation of the lungs. Inflammation of the lining of bronchial tubes causes COPD, and it causes the cells to multiply rapidly to repair the damage. Rapid multiplication may lead to mutation, causing them to develop into cancer.
Genetic Risk:
A genetic assessment can help determine who develops lung cancer and COPD.
Age:
Older people are more likely to develop both conditions because the body can’t repair DNA damage as effectively as in a younger body.
Studies show the prevalence of COPD in people aged 65 and older is 14.2% compared to 9.9% in those who are 40+ years.
However, it’s important to note that having COPD doesn’t mean you’ll develop lung cancer; it only increases the risk.
A controlled study to assess the risk of developing lung cancer in patients with COPD within ten years found a probability of 8.8% for those with COPD to get lung cancer compared to 2% in patients with normal pulmonary function.
The treatments for lung cancer and COPD are also different. The doctor may prescribe anti-inflammatory drugs, lung surgery, and extra oxygen to treat COPD and radiation and chemotherapy for lung cancer.
Can You Live a Normal Life With COPD?
Although COPD has no cure, patients can live a normal life. With medication, a good diet, and proper care, you can manage the challenges of living with COPD.
Here are some tips:
Quit Smoking:
Smoking is the leading cause of COPD and cessation goes a long way in improving one’s quality of life. Prescription drugs, nicotine gums, vapes, and patches may ease the process.
Pay Attention to How You Breathe:
COPD may have damaged the lungs and reduced their springiness, so there isn’t enough oxygen in the blood. As a result, breathing becomes difficult, causing you to huff and puff when walking, running, or performing other sub-aerobic activities. You can incorporate breathing exercises into your routine to increase oxygen in your system. Tools like pacers help you to take deep, slow, and gentle breaths while moving at your pace to keep breathing under control.
Eat Healthy:
With COPD, the body uses more energy to breathe, increasing its nutritional demands. Good nutrition provides enough energy while keeping opportunistic infections at bay. Studies show a Mediterranean diet rich in plant foods and healthy fats helps improve lung function, while a diet rich in saturated fat, sugar, meat, and salt worsens the condition.
Exercise:
Keeping physically active is also crucial for COPD patients. Studies show exercise is essential in pulmonary rehabilitation for people with lung-related diseases. It improves oxygen production in the body, increases energy levels, and strengthens the lungs and the heart, which reduces shortness of breath. Cardiovascular exercises like walking, hiking, jogging, and strength training using resistance bands help minimize the severity of the condition.
Prognosis – How Much Time You Have Left
Since COPD shortens one’s life expectancy, knowing how much time you’ve left is important. Typically, the period varies from one person to another depending on their overall health and if they have other diseases.
Your doctor will likely recommend that you have a pulmonary function test (PFT) to determine how well your lungs are working and whether your COPD treatment plan is working.
With the pulmonary function test results, your doctor may use that information to aid in determining what stage your COPD is in.
In combination with pulmonary function tests, the two most commonly used methods to measure the severity of COPD is the GOLD System and the BODE Index.
GOLD System
The GOLD (Global Initiative for Chronic Lung Disease) system determines the extent of the illness by classifying COPD in grades. GOLD is a group of lung health experts who formulate the guidelines doctors must use when treating COPD patients.
GOLD uses the forced expiratory volume (FEV1) test from your pulmonary function test to categorize the severity of COPD into stages.
The forced expiratory volume (FEV1) shows the amount of air a person can forcefully exhale in one second.
COPD has four total stages, and your airflow becomes more limited with each stage
Here are your numbers and how the GOLD System breaks down the COPD Stages:
- Stage 1: Very mild COPD with a FEV1 about 80% or more of normal.
- Stage 2: Moderate COPD with a FEV1 between 50 and 80% of normal.
- Stage 3: Severe emphysema with FEV1 between 30 and 50% of normal.
- Stage 4: Very severe COPD with a FEV1 of <30%, or those with Stage 3 FEV1 and low blood oxygen levels
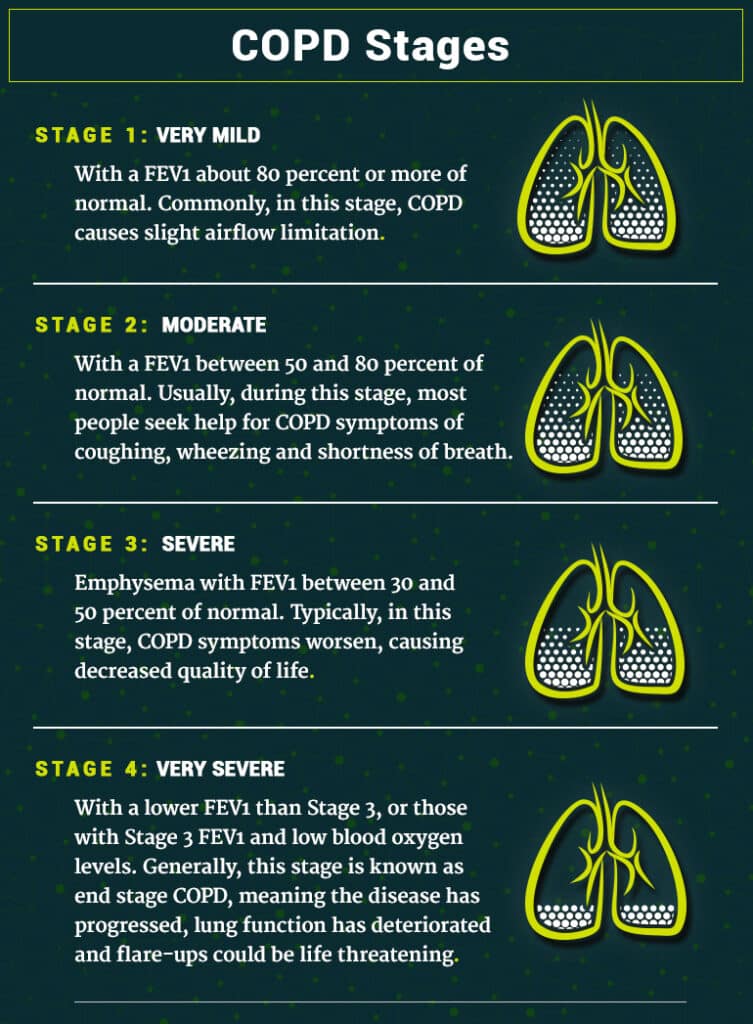
Simply put, as the COPD Stage numbers increase, the lung prognosis and life expectancy with COPD worsens.
The doctors also assess the patient’s symptoms, number of flare-ups, and exacerbations that need hospitalization. As discussed earlier, patients are then classified into four groups (A, B, C, D). This means a COPD patient labeled GOLD Grade 4, and Group D has a shorter life expectancy than one in GOLD Grade 1, Group A.
BODE Index
Other scientists came up with the BODE Index to measure the severity of COPD.
This is another measure used to evaluate a patient’s COPD condition. BODE takes on a more holistic view of the patient by measuring their body mass (BMI), airflow obstruction, dyspnea, and exercise capacity.
The BMI measures the patient’s body mass based on their weight and height to determine if the person is overweight or too thin, while an FEV1 score is allocated to determine if they have airflow obstruction. BODE Index also shows if the patient has difficulty breathing (dyspnea) and if they can tolerate exercise using a six-minute walk test (exercise capacity).
BODE stands for body mass, airflow obstruction, dyspnea, and exercise capacity.
The BODE Index accounts for how COPD affects your life.
- Body Mass
- Airflow Obstruction
- Dyspnea
- Exercise Capacity
The body mass index (BMI) helps determine if you’re overweight, obese or underweight.
Airflow obstruction refers to your FEV1, which is similar to the GOLD system.
Dyspnea means trouble breathing, and exercise capacity refers to exercise tolerance. Many people with COPD take a six-minute walk test—the distance you can walk in 6 minutes—to evaluate their level of exercise tolerance.
These combined measurements comprise the BODE Index and can be used to put COPD into stages or approximate life expectancy with COPD.
Get Routine Blood Tests
Routine blood tests help identify specific inflammation biomarkers that show the severity of COPD in the patient. Examples of biomarkers are blood eosinophils (B-Eos) and neutrophil-to-lymphocytes (NLR).
A study published in the International Journal of Chronic Obstructive Pulmonary Disease shows that patients with COPD have an elevated level of NLRs or B-Eos.
Look at COPD Mortality Rates
As earlier highlighted, COPD reduces a patient’s life expectancy depending on the stage of COPD. Patients with stage 1 COPD shorten their life expectancy by 0.3 years, stage 2 by 2.2 years, and stage 3 by 5.8 years.
This is an excellent basis to determine the amount of time a patient has to live. Moreover, if the patient is still smoking, they reduce their life by 3.5 years.
Once on Oxygen
As COPD worsens, the patient becomes a potential candidate for oxygen therapy because the body is probably not getting enough oxygen on its own.
Oxygen therapy provides supplemental oxygen to protect your organs from damage, improve your quality of life and prolong your life.
The supplemental oxygen may be administered using an oxygen tank, facemask, tubes (or nasal cannula), or surgery.
How To Extend Your Life With COPD
You can still extend your life even when diagnosed with COPD. Here’s how to do it:
Early Diagnosis Can Make a Difference
COPD is the most underdiagnosed and undertreated disorder, especially during its mild and moderate stages.
A study by Laucho-Contreras and Cohen-Todd shows that 85% of COPD patients had consulted their doctors for respiratory problems over the last five years before the diagnosis.
Early detection helps manage the symptoms, but since most cases are underdiagnosed, many doctors identify the problem when it’s too late.
An early diagnosis happens when the patient has exhibited two registered indicators in the last five years before COPD diagnosis.
Such a diagnosis encourages the patients to stop smoking, increases the patient’s life expectancy, and creates an opportunity for COPD medication to work before the condition progresses to more severe stages.
However, if the condition is diagnosed late, the patient will likely exhibit more than three indicators.
Such indicators include:
- Pneumonia
- Prescription of oral steroids
- Other respiratory diseases other than pneumonia
- Antibiotic prescription to open the airway and manage lung infections
Late diagnosis delays treatment and any intervention to stop smoking. Moreover, the damage to the lungs and the airways may be so severe it becomes impossible to reverse.
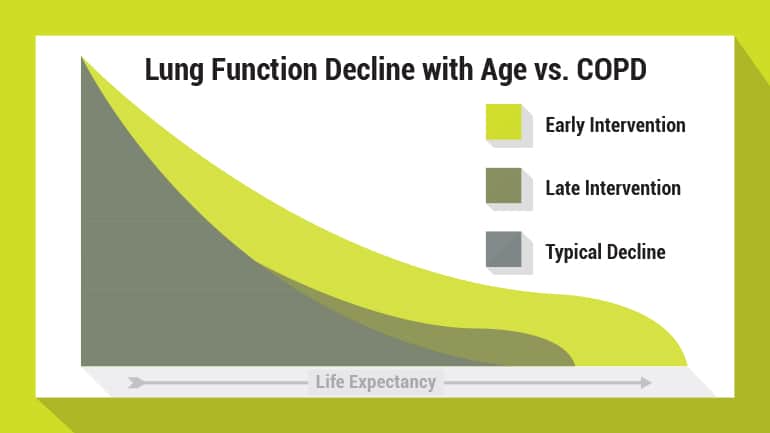
COPD Life Expectancy Chart
The below COPD Life Expectancy chart shows how lung functions decline with age vs with COPD and how early or late intervention can increase or decrease your life expectancy.
Making Lifestyle Changes
Lifestyle changes help manage COPD symptoms and improve overall health, thus extending your life.
Your doctor may recommend a pulmonary rehabilitation program where a team of specialists prescribe breathing exercises, provide nutrition advice, and physical exercises to enhance the quality of life.
They’ll also provide guidelines to help you stop harmful habits like smoking.
Since COPD makes you vulnerable to infections like pneumonia and influenza, the program will include vaccination for pneumococcal disease and flu.
Is Medication Available?
Doctors also prescribe medication to help reduce airway inflammation, reduce bacterial infections, and open up blocked airways. Common types of medications prescribed are:
Bronchodilators:
The medicines widen the airways to ease breathing and minimize the number of flare-ups if COPD worsens.
The doctor will probably prescribe an inhaler or use a combination product like short-acting beta-agonists, methylxanthines, or anticholinergic bronchodilators.
Short-acting beta-agonists are prescribed if the symptoms occur occasionally, e.g., when exercising. They also prevent a full-on attack when you experience shortness of breath.
Methylxanthines are prescribed when the patient has difficulty using an inhaled medication, while anticholinergic bronchodilators ease breathing.
Antibiotics:
If the body has developed a bacterial infection in the respiratory tract, the doctor will prescribe antibiotics to treat it.
Daliresp:
The drug is formulated for patients with chronic bronchitis and is administered to prevent COPD flare-ups.
Corticosteroids:
These drugs reduce inflammation in the airways and are prescribed when bronchodilators alone can’t manage COPD symptoms effectively.
Final Thoughts
Although COPD life expectancy reduces significantly over time, it’s possible to live a healthy life. Early diagnosis helps embark on treatment when medication is most effective while encouraging you to stop harmful habits like smoking.
When coupled with other remedies like breathing exercises, healthy nutrition, and lifestyle changes COPD patients can live longer regardless of the group or stage of COPD.
Remember, always discuss your medical conditions and treatment options with your doctor.

Christine Kingsley, APRN is the Health and Wellness Director at the Lung Institute where she focuses on providing helpful online resources for people looking for information on various lung diseases, breathing exercises, and healthy lifestyle choices. She advocates for holistic care that involves working with your doctor to explore all options including traditional and alternative care while focusing on diet and exercise as proactive measures.









