What is Pulmonary Fibrosis?
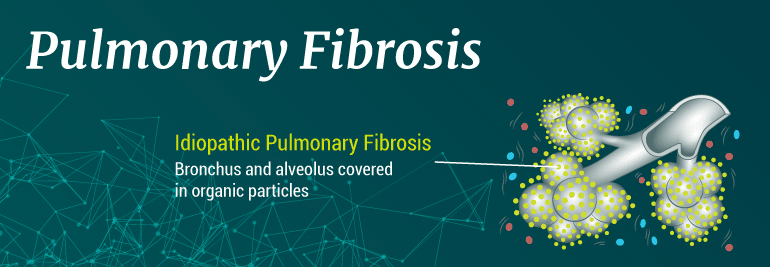
Pulmonary fibrosis is a lung disease that scars the lungs, causing intricate pulmonary passageways to thicken and harden and obstructing the free passage of oxygen through the walls of the lungs’ tiny air sacs (alveoli) into the bloodstream. The resulting lack of oxygen in the bloodstream leaves pulmonary fibrosis sufferers short of breath even after periods of prolonged rest. Idiopathic pulmonary fibrosis is a form of pulmonary fibrosis with no known cause.
Pulmonary fibrosis is a progressive disease that varies in the rate of degeneration from person to person. This condition is part of a group of conditions referred to as interstitial lung disease.
The term interstitial lung disease refers to conditions that lead to inflammation or scarring of the lung’s delicate tissues. Some autoimmune disorders, specifically connective tissue disorders like rheumatoid arthritis can cause interstitial lung disease.
Scarring of the lungs is irreversible, and there is no cure for pulmonary fibrosis. However, treatment options are available.
Who can develop pulmonary fibrosis?
Idiopathic pulmonary fibrosis has no specific demographic. However, it does affect men more than women. It typically occurs in individuals between the age of 50 and 70, and has an increased risk for individuals who smoke cigarettes.
Researchers are still studying to determine a specific cause of this condition.
Symptoms of pulmonary fibrosis
The symptoms of pulmonary fibrosis differ by individual, but the most common symptoms include:
- Shortness of breath
- Dry, chronic cough
- Fast breathing
- Constant fatigue
- Aching joints and muscles
- Clubbing (widening and rounding) of the fingers and/or toes
These symptoms are indicators that you may have pulmonary fibrosis or a similar condition. If you are experiencing any or all of these symptoms, you should schedule an appointment with your doctor to determine the cause of your symptoms and the treatment options available to you. Often, your doctor will walk you through a simple diagnosis to determine if you have pulmonary fibrosis or a similar condition.
Diagnosing pulmonary fibrosis
Once you make an appointment with your doctor to determine if you have pulmonary fibrosis, your doctor will walk you through a couple diagnostic tests. Each patient is different, and you may not require all of the steps in the diagnosis process.
A typical pulmonary fibrosis diagnosis includes the following tests:
- A conversation with your doctor about your family’s medical history
- A question session about your medical history and lifestyle choices
- A physical examination where the doctor listens to your lungs
- A pulmonary function test that measures your lung capacity and function
In some cases, a doctor may recommend an X-ray and lab work to determine the severity of your condition. Pulmonary fibrosis, like most chronic lung diseases, is a progressive condition that worsens over time. Before your doctor can accurately recommend treatment, he or she must identify the severity of your condition.
Treatment options for pulmonary fibrosis
Typically, patients who have been diagnosed with pulmonary fibrosis do not live more than five years after a diagnosis. However, there are new treatment options available that can not only help reduce your symptoms when they occur, but they can also help to slow the progression of your disease.
Most doctors recommend traditional treatment for pulmonary fibrosis. Traditional pulmonary fibrosis treatment helps lessen your symptoms when they occur, but it does not prevent them from occurring. These treatments focus more on maintenance than prevention. For example, an inhaler is one of the most common methods of pulmonary fibrosis treatment. An inhaler helps to open your airways in the midst of an airway attack when you cannot get enough air into your lungs. It doesn’t prevent you from having the attack to begin with.
This is the case for most of the traditional treatments available for pulmonary fibrosis, such as:
- Steroid or other medications
- Inhalers
- Oxygen therapy